Platelet Rich Plasma (PRP) Therapy
A short history of Wound Healing and PRP
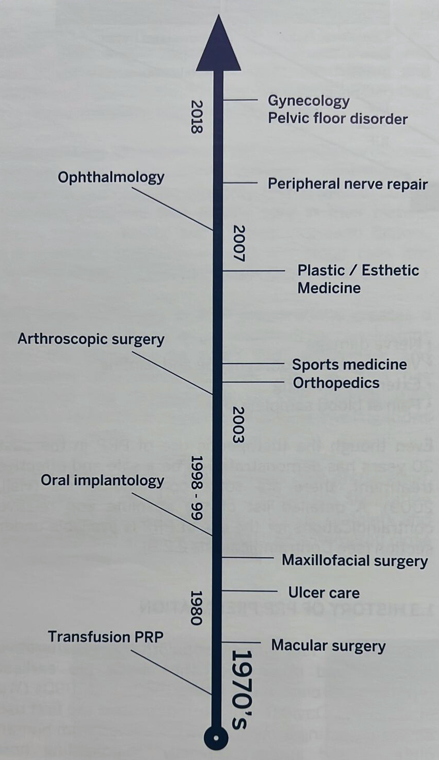
In the literature, PRP has gone from strength to strength since reports of its earliest use in the 1980s and 1990s
David Knighton first decried it as “locally acting growth factors obtained friend from human platelets and applied topically”. Then, laboratory tubes were used without any polymer-based separating gel.
The Maxillofacial surgeon Dr Robert Marx evaluated the effects of PRP on bone maturation rates and bone s=density grats in reconstructions of mandibular continuity defects. Addition of PRP led to increased bone formation.
Following flow diagram shows the diffusion of PRP use into different specialities. (Pg 14 Regenkit book)
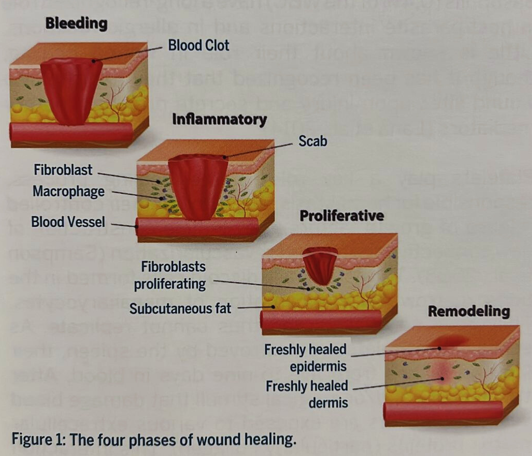
Basics of Wound healing and Role of different blood components in PRP
(Pg 9 Regenkit book)
Definition of PRP: PRP is retrieved from a patient’s whole blood and centrigued to obtain high concentration of platelets, working definition is platelets > 1,000,000 platelets/ microLitres .
Depending on the system utilized, most PRP systems commercially available give a concentration of 4-8x that of peripheral blood.
Although it seems intuitive that there would be a linear dose-response relationship, extremely high doses of platelets decreased angiogenesis.
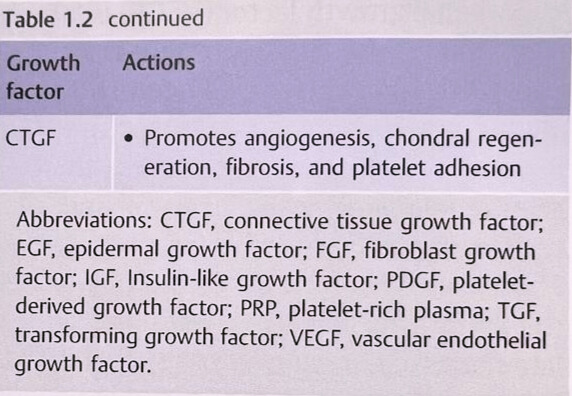
Platelets contain more than 20 different types of growth factors in their Alpha granules. The following table lists some of them:
(Thieme Pg 5)
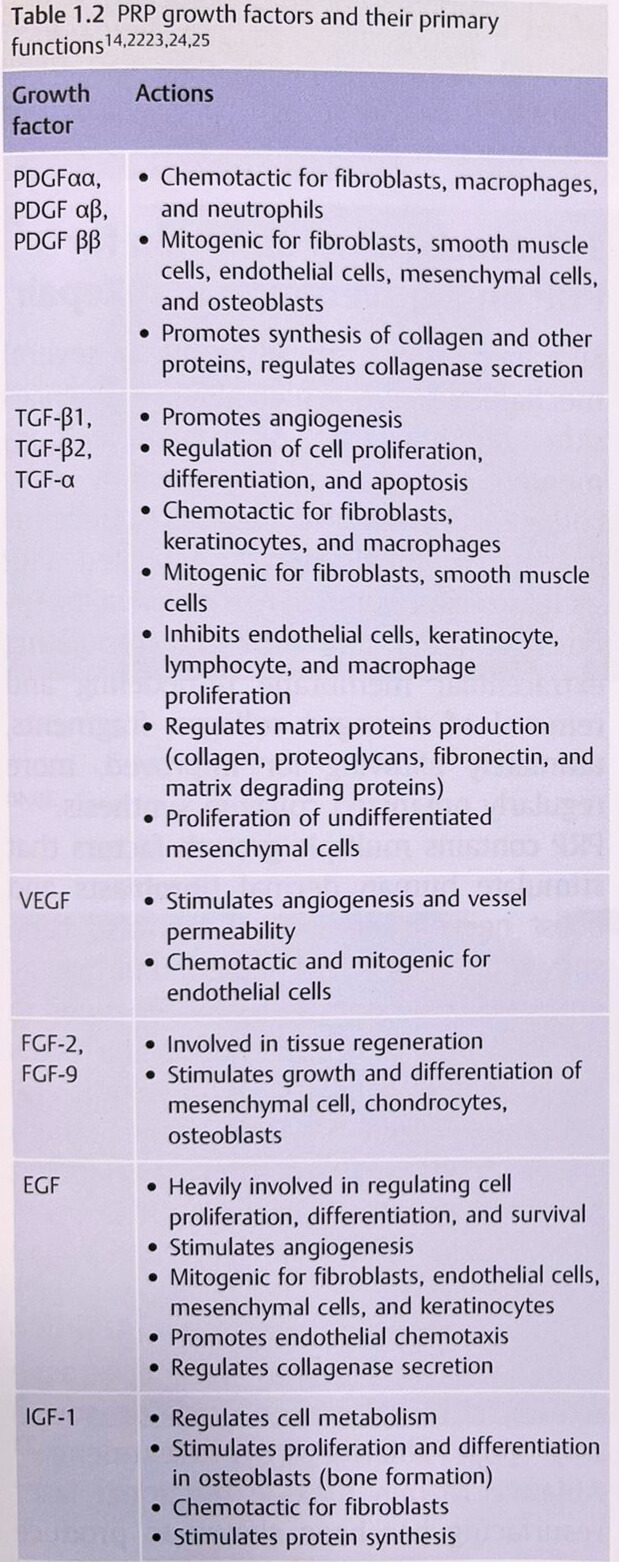
Platelets secrete most of their growth factors within an hour upon activation, with the rest being released for up to 7 days. PRP increases release of cytokines , which bind to the surface of cellular transmembrane receptors, effecting intracellular signalling. Changes at te microscopic level include 1) angiogenesis 2) collagen synthesis 3) ECM production 4) decreased apoptosis.
All these effects basically mirror the mechanisms required for its widespread Dermatological, Orthopaedic and other uses.
- From Bench to Bedside:
- Case studies for a wide variety of Clinical Indications
- Wound Healing: ulcers and Post Laser/ Microneedling with Fractional RF (MNFRF) therapies etc
- Hair Growth especially Alopecia areata and AGA
- Aesthetic and Cosmetic Dermatology: Rejuvenation and Augmentation
- Plastic Surgery: enriching Autologous Fat Grafting ; PRP and Fibrin
- Urology : increasing Erectile function, especially in Peyronie’s disease and ED
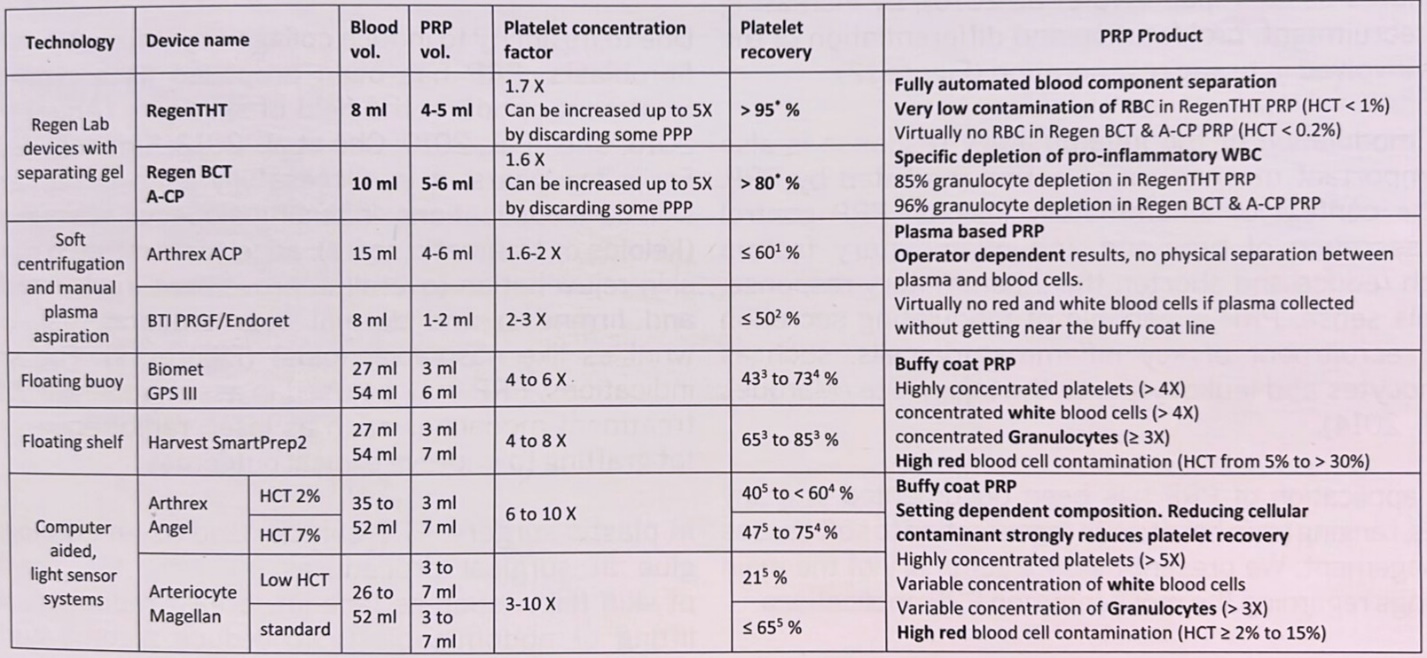
Overview of PRP systems:
(Regenkit Pg 15 Table 1)
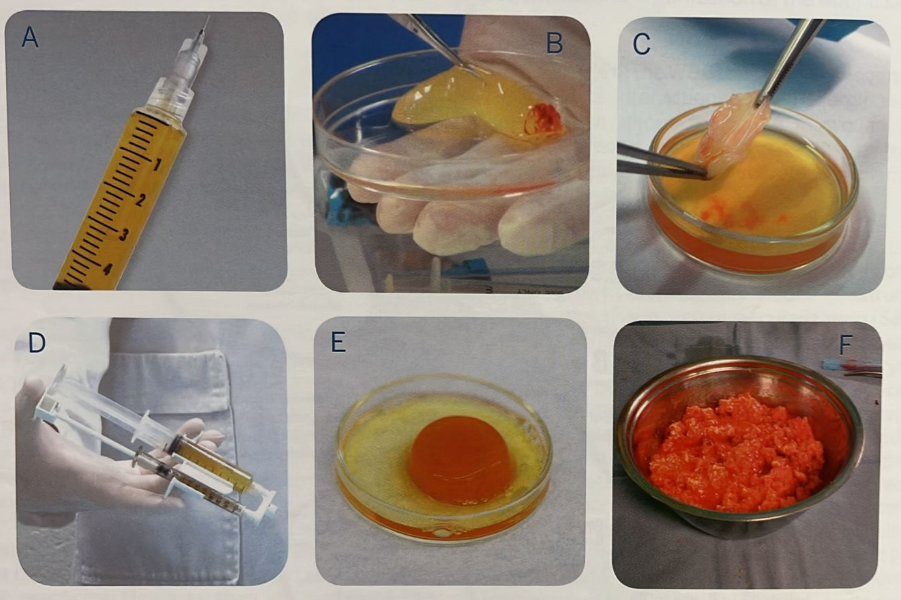
(Different forms of PRP obtained from Regenkit Book Pg 12)
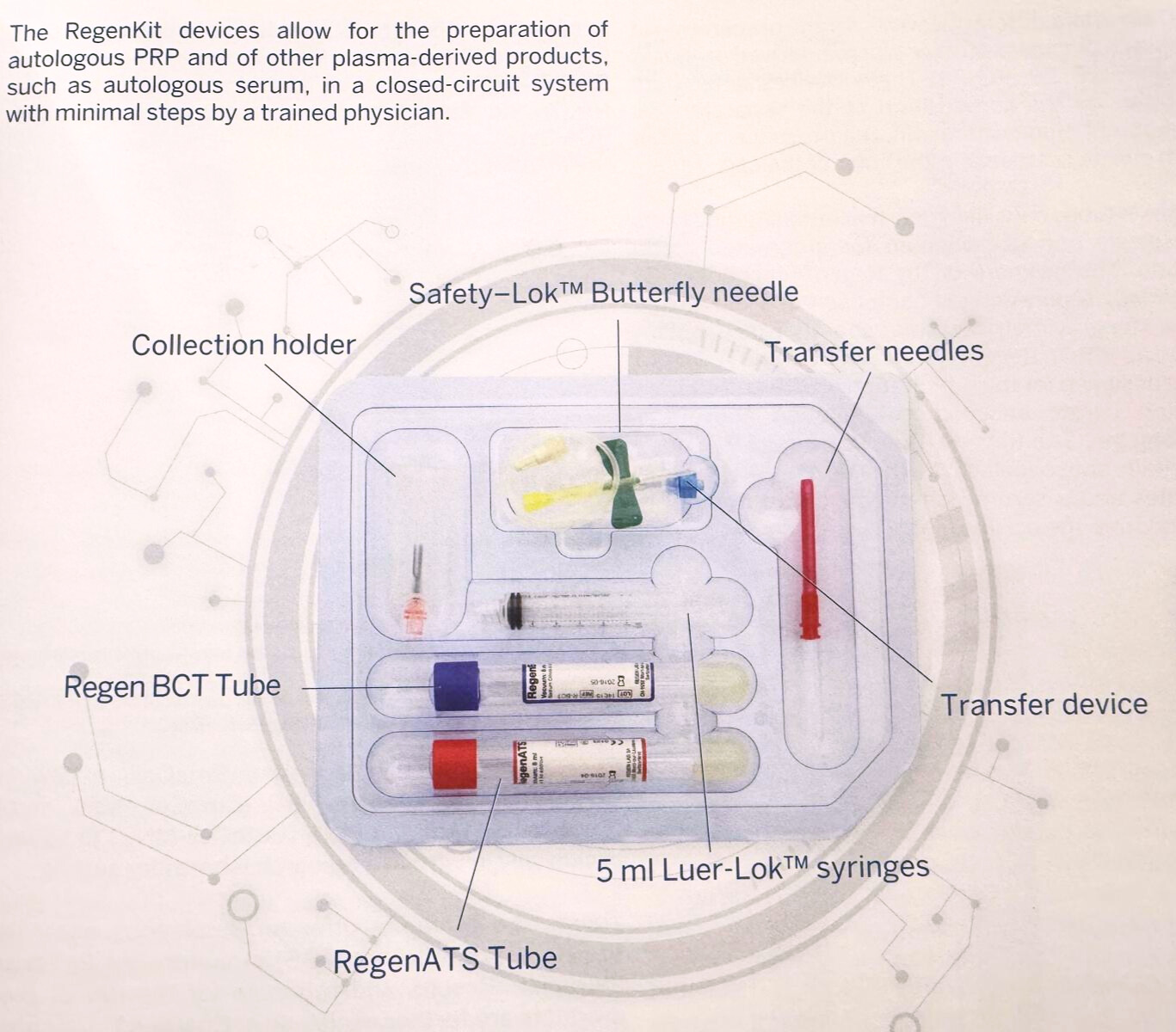
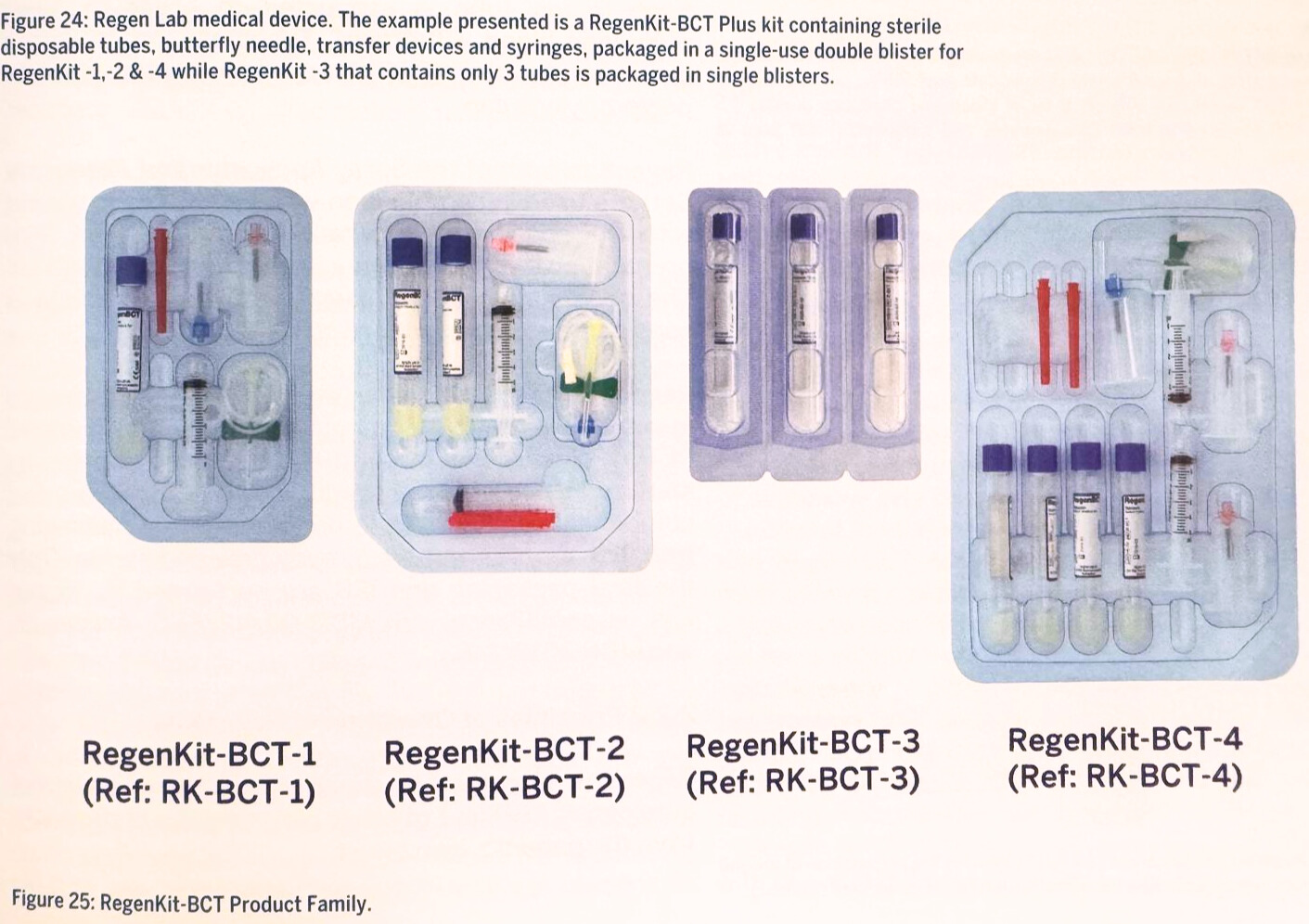
Focus on one widely available system in South East Asia –
The RegenKit
(Regenkit book Pg 41)
Tests of active components using ELISA kits Eg from ThermoFisher
Ref: Cole et al – Stem Cell Investigation 2017;4:88
Overview of whole blood vs PRP
- Future directions and Indications
Since wound healing (due to a variety of bodily insults or ageing processes) are common features of a whole cross-section of Human health, we at ASRM only foresee the uses of PRP as EXPANDING into the future
The challenges are standardizing PRP extraction and reinjection procedures (image-guided or otherwise), PRP has already been combined with Hyaluronic acid with good results (especially in Cosmetic and Orthopaedic procedures). Similar results have been reported with combinations of Autologous fat.
Future directions may include the combination with Exosomes etc.
The future is BRIGHT, and it behoves us in Asia to contribute to this established , exciting and promising therapy.